The concept of dissipated energy in mechanical ventilation is crucial, especially in understanding how different ventilation strategies might affect the lung tissue, particularly in patients with compromised lung function. Flow-controlled ventilation (FCV) aims to optimize the mechanical energy delivered to the lungs to reduce ventilator-induced lung injury (VILI). Here’s how FCV addresses energy dissipation compared to conventional ventilation modes:
Energy Dissipation in Mechanical Ventilation
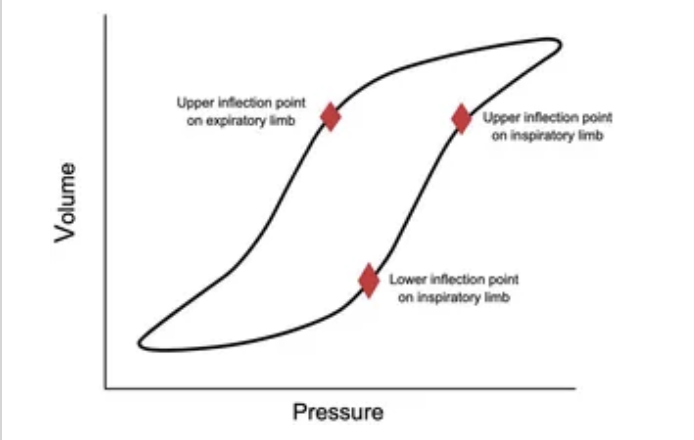
Dissipated energy in the context of mechanical ventilation refers to the energy that is not stored elastically within the lung tissue but is lost through resistive processes such as airway resistance and tissue damping. This energy contributes to lung stress and strain, which can exacerbate or lead to VILI.
How FCV Modulates Energy Dissipation
1. Constant Flow Delivery:
• FCV provides a steady flow of air into the lungs throughout the inhalation phase. This constant flow reduces the peaks in flow rate and pressure that are characteristic of conventional modes like volume-controlled ventilation (VCV) or pressure-controlled ventilation (PCV).
• By reducing these peaks, FCV minimizes the high instantaneous power transfers that occur when a large volume of air is pushed into the lungs in a short period, which can overdistend alveoli and increase the risk of lung injury.
2. Reduced Airway Pressure Fluctuations:
• The constant flow characteristic of FCV results in a more linear and predictable increase in airway pressure during the breath cycle. This contrasts with VCV, where pressure can peak sharply depending on the compliance of the lung and the set tidal volume.
• By moderating pressure fluctuations, FCV can help maintain a more uniform transpulmonary pressure, potentially reducing the risk of barotrauma and volutrauma.
3. Enhanced Gas Exchange Efficiency:
• FCV can improve the efficiency of gas exchange by maintaining a more consistent and adequate alveolar ventilation throughout the respiratory cycle. This consistent ventilation helps avoid areas of hyperinflation and atelectasis, promoting more homogeneous lung inflation.
• This homogeneous distribution of gas may lead to improved oxygenation and CO2 removal while using lower overall energy inputs.
4. Potential for Reduced VILI:
• With FCV, the lower variability in flow and pressure reduces the mechanical load on lung tissues during each breath cycle. This reduction in cyclic loading can decrease the mechanical stress on the lungs, lowering the risk of VILI.
• The gentler, more consistent inflation pattern may help protect the lung’s delicate structures, especially in patients with ARDS or other forms of severe lung injury, where even small reductions in additional lung stress can significantly impact outcomes.
Clinical Implications
While the theoretical benefits of FCV in terms of energy dissipation are compelling, clinical evidence is still developing. Preliminary studies and trials are needed to quantify these benefits fully and understand how they translate into improved clinical outcomes such as reduced incidence of VILI, shorter durations of mechanical ventilation, and better overall survival rates in critically ill patients.
Overall, FCV offers a promising approach to mechanical ventilation that could potentially align better with lung protective strategies by minimizing energy dissipation and reducing lung stress and strain during critical care.